Common (medical) testing of the bowel -what the tests involve and why they are done
18 Oct 2023

Common bowel tests: what they involve and why they are done
Have you ever wondered what happens during testing of the bowel? And why these tests are performed? This Australian Physiotherapy Association article outlines the various medical tests relating to bowel function/dysfunction, including the rectum and anal sphincter muscles.
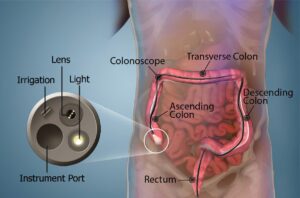
Colonoscopy
How is it performed?
A colonoscopy involves passing a long, thin, flexible tube (a colonoscope) which has a tiny camera on the end, through the anus to look inside the rectum and colon (lower part of the bowel). Before having a colonoscopy, the patient will be given strict instructions on bowel preparation beforehand to clear bowel contents, which will usually include fasting, drinking a bowel prep and the use of an enema. They will generally be under moderate or deep sedation during the procedure. While a colonoscopy can just involve looking inside the colon and rectum, often a biopsy (typically of a polyp), is taken for further laboratory analysis or an internal haemorrhoid may be banded during the procedure. This video shows the procedure in animated form.
Why is a colonoscopy performed?
A colonoscopy is typically done to look for any abnormalities in the rectum and colon. This can include haemorrhoids, polyps (which can be harmless but are sometimes pre-cancerous), cancers, diverticulitis, Crohn’s disease, or ulcerative colitis. Typically, a colonoscopy will be performed to investigate reasons for the patient’s particular signs or symptoms (e.g. if they have bleeding, chronic diarrhoea, or pain, to see if an obvious cause can be found). Colonoscopies are also performed as a screening investigation (e.g. if the patient has a strong family history of bowel cancer, or if they have a past history of disease themselves).
How are the results presented?
The results will be presented in a written report. Look out for any of the problems mentioned above. Sometimes photos taken during the procedure will be included.
Sigmoidoscopy
How is it performed?
A sigmoidoscopy is very similar to a colonoscopy, but the thin, flexible tube (sigmoidscope) only goes as far as sigmoid colon, rather than further up into the colon. The patient still needs to do an enema before the procedure, but not a full bowel prep. However, it can be done under no or very light sedation.
Why is a sigmoidoscopy performed?
A sigmoidoscopy is performed for very similar reasons as a colonoscopy but may be done instead if it is suspected that the patient’s problems are isolated to the rectum or sigmoid colon, or in patients under 50 where any bright red bleeding is most likely to come from haemorrhoids or fissures in this region.
How are the results presented?
A written report will be provided with the findings.
Endoscopy
How is it performed?
An endoscopy involves passing a long, thin, flexible tube with a tiny camera on the end through the mouth and into the oesophagus, stomach, duodenum and upper part of the small intestine. The patient will need to fast for a period of time before an endoscopy and is usually under deep sedation.
Why is an endoscopy performed?
An endoscopy may be performed to investigate causes for symptoms such as pain, vomiting, bleeding, nausea, heartburn and difficulty swallowing, where the problem is thought to be in the upper section of the gastro-intestinal (GI) tract. The surgeon will typically be looking for abnormalities in tissues of the upper GI tract, such as polyps, cancers or ulcers. A biopsy may be taken if the patient has suspected helibactor or coeliac disease, polyps removed, or bleeding vessels cauterized. If there is an object causing an obstruction, such as a swallowed foreign body, this will be removed.
How are the results presented?
A written report is typically given, but sometimes it will include photos.
Endoanal ultrasound
How is it performed?
An endoanal ultrasound transducer is a thin probe, about the width of a finger, which gives a 360 degree cross-sectional view (or more recently now a 3D view) of the muscles and tissues in the anus. The patient usually lies on their side for the procedure, and the probe is inserted approximately 5cm into the anus. The patient does not need to be sedated for the procedure. It is a fairly quick test, taking 10-15 minutes to perform.
Why is an endoanal ultrasound performed?
This procedure is usually done to check if the anal sphincter muscles (internal anal sphincter [IAS] and external anal sphincter [EAS]) are physically damaged in people with symptomatic faecal urgency and/or faecal incontinence. This may be because the patient has symptoms, or it may be sometimes performed if the patient has had a high-risk birth (e.g. with a high level 3 degree or a 4 degree tear) to check the extent of sphincter damage. An endoanal ultrasound can reveal defects and the extent of the defect in the IAS or EAS muscles.
How are the results presented?
You may get a written report with the conclusions of the endoanal ultrasound, but it can also be really useful to be able to interpret the ultrasound images themselves. There will often be a series of images taken at different levels inside the anus, which look like a series of black and white rings. The report will refer to different segments like reference points on a clock – where 12 o’clock is the top (most anterior aspect), 6 o’clock the most posterior aspect, 3 o’clock on the left side and 9 o’clock on the right hand side.
The central black circle surrounded by a very clear, thin, white and black circle are just from the probe itself. The first ‘fuzzy’ area of white tissue encircling this is the submucosal tissue. External to this is another circle of black or grey, which is the IAS. You may not see this if the image is taken from the very lowest part of the anus but it should be clearly defined and continuous in the mid to upper anus. Any break in the continuity of this circle (represented by white areas breaking up the dark circle), or changes in thickness in different parts of the circle can indicate IAS damage.
The EAS is external to the IAS and is represented by the outer-most fuzzy white area. It should be continuous. Watch out for changes in thickness and gaps in the continuity of this circle (represented by dark areas where it should be white), as this can indicate areas of EAS damage. However, be aware that images taken in the upper anus, near the ano-rectal junction can make it appear as if the EAS is damaged anteriorly, when in reality, this is part of the normal anatomical junction where the EAS ends and the puborectalis muscle begins (showing up as white areas to the sides and posterior aspect of the anus/rectum, where it loops around the anus). Have a look online if you are unfamiliar with endoanal ultrasound results as you will find numerous examples, such as this source showing IAS and EAS defects.
Ano-rectal manometry
How is it performed?
Ano-rectal manometry involves the insertion of a very thin, flexible tube with a small balloon on the end (which is deflated on first insertion), into the anus and rectum at various depths. Like the endoanal ultrasound, the manometry catheter has circumferential pressure sensors all along its length at 1mm intervals, to take pressure measurements in many different areas at once. The patient usually lies on their side and does not require sedation.
Initially, the device will measure resting pressure in the anus and rectum. Then the patient is typically asked to do various things, including squeeze and relax their anal sphincters for various amounts of time, strain and cough. The balloon may also be inflated to check for sensation, the recto-anal inhibitory reflex (RAIR) or the ability to expel the balloon, depending on what the doctor is looking for.
Why is ano-rectal manometry performed?
This is another test of the anal sphincter muscles but this time testing for their function and coordination. Manometry may test if the sphincter muscles can contract appropriately and if the strength is normal, when squeezing or coughing (e.g. for investigation of muscle function in those with faecal urgency or incontinence). It can also test if the muscles relax appropriately after contraction, and when straining or defecating, in those with obstructed defecation or constipation. In can be very useful to diagnose problems with muscle or nerve function (e.g. after surgery or in diseases such as Hirschsprung’s) and will show up abnormalities in reflexes such as in the RAIR.
How are the results presented?
Ano-rectal manometry results will include a series of coloured images, each representing a different stage of the test, often with written comments for each image. When looking at the images, it is important to know what was being asked of the patient at each stage (e.g. was the image taken at rest or on squeeze). The upper half of the image represents pressure in the rectum, and the lower half represents pressure in the anus from upper to lower aspects (with the bottom of the image being the outside). The warm colours on images (dark red, red and orange), represent areas of greater pressure, with cooler colours (green and blue), representing areas of low pressure.
Depending on the stage of the test you would expect to see different colours and patterns. For example, when squeezing, we should ideally see a block of red or orange in the anal region, that is well sustained. When relaxing, we should see lighter colours in this same region. When straining, we may see an increase of pressure (warm colours) in the rectum but a decrease in pressure (cool colours) as the anus relaxes. There can be many types of abnormalities, which can include only very light colours (reduced pressure), on attempts to squeeze, or a lot of red/dark red colour (high pressure) when at rest or trying to empty the bowel. This free access paper shows some of the images you could see on ano-rectal manometry testing.
Defecating proctogram
How is it performed?
A defecating proctogram involves insertion of a barium-containing paste (which will show up on an X-ray), into the rectum. The patient is then asked to sit on a special toilet behind a screen, and real-time X-rays (fluoroscopy) are taken of the bowel as the barium paste is evacuated. Patients may be asked to squeeze and hold the paste in before emptying, or to strain as they empty. Functional magnetic resonance imaging (FMRI) are sometimes used to do the same procedure now, in which case, the patient will be semi-recumbent with their knees drawn up.
Why is a defecating proctogram performed?
A defecating proctogram can be used to show what happens in real-time as the patient is passing a bowel motion (albeit in far from normal conditions). The fluoroscopic images will show the passage of the paste, and thus also show what happens to the bowel wall and pelvic floor muscles during defecation. This is helpful when diagnosing evacuation disorders to help show the source of the problem (e.g. a rectocele vs. an intussusception when planning for surgery). A defecating proctogram may also highlight functional defecation disorders, such as excessive pelvic floor relaxation and stretch, or alternatively pelvic floor muscle dyssynergia or anismus during the defecation process. This can help to target treatment. Due to the abnormal conditions of the testing process, some argue that a defecating proctogram may tend to over-diagnose conditions such as anismus or pelvic floor dyssynergia.
How are the results presented?
The results will generally include a written report and accompanying fluoroscopic images (or sometimes a video). The images or video will be black and white showing a sagittal view of the rectum and anus. The barium paste will show up as darker on the image, helping to highlight its passage and hence also the surrounding walls of the rectum and anus. You can find some videos online of defecating proctograms, such as this example.
Hopefully this helps you to understand a little more about various bowel tests, what they involve and why they are performed. I would encourage you to build relationships with your local colorectal surgeons to help you learn more in this field and better help your patients.

